We’re committed to keeping our readers informed.
We’ve removed our paywall from essential coronavirus news stories. Become a subscriber to support our journalists. Subscribe now.
Throughout the pandemic, wearing a face mask has been one of the best ways that anyone can easily reduce their risk of catching or spreading COVID-19. Putting aside the often contentious debate over mask mandates, face masks remain a crucial and effective individual tool, which is why it continues to be frustrating that most people, two years in, are not wearing better masks. That’s due in large part to mixed messaging from public health officials — the CDC only recently began emphasizing the importance of higher filtration masks — but the bottom line is that the cloth masks everyone started buying in the spring and summer of 2020 were never a great match for an airborne virus like COVID and are even less so against more transmissible variants like Delta and Omicron. Surgical masks, when medical-grade quality and worn tightly across the face, are better than cloth masks. But high filtration respirators like N95s or KN95s — which are quite comfortable and have been widely available from reputable sellers in the U.S. for a long time — are what everyone should now be using and what every institution should be making available.
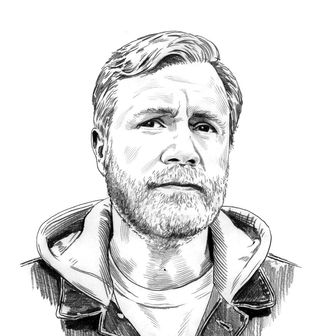
One of the most vocal advocates for the use of higher-quality masks throughout the pandemic has been Stanford infectious-diseases doctor Abraar Karan, who has researched COVID transmission and been calling for the use of high-filtration masks since the spring of 2020. His Twitter feed continues to be an invaluable resource for information on mask effectiveness, criticism of the inadequate public-health efforts regarding masking, and other commentary on COVID-19. I spoke with Dr. Karan about his ongoing campaign for better masks, their importance in the fight against Omicron, and why you should replace that cloth mask in your underwear drawer.
Why should people start using high-filtration masks like N95s and KN95s as their go-to, everyday masks rather than cloth ones?
The key reason is that transmission of the coronavirus is primarily through aerosols, which float around in the air — you inhale them — and are not filtered well by cloth masks. You really need melt-blown polypropylene, which you find in surgical masks and N95s, to stop these small particles.
So the materials used to make these masks make them better equipped to filter out the virus?
Yeah. The material is basically melt-blown polymers, like polypropylene, which form this complex sort of webbing which is then electrostatically charged, and that pulls the particles in when you’re inhaling and exhaling. Cloth masks are often just woven thread and other materials that don’t have that design. Cloth masks don’t provide great source control, either. The CDC is now letting people who test positive for COVID-19 stop isolating after five days and then wear a mask for five days. It would have been ideal for them to also recommend that be a better mask.
So do you think normal people should get N95 or KN95 respirators and then throw out their cloth and surgical masks?
I think the surgical masks can still work really well with a mask fitter [i.e., a frame or brace that is worn over the mask, ensuring an improved fit]. Surgical masks are also melt-blown polypropylene, three layers. They’re actual medical three-layer masks. So those are still pretty good if you can get the fit improved. In terms of cloth masks, I’d rather you wear something than nothing. But if you’re able to upgrade, that would be great.
As one of my colleagues has put it, just like you have a fire extinguisher, everyone should have access to respirators for an emergency. And I think that’s right. I think that the next time there’s a pandemic, or the next surge or whatever it is, if we need to wait for new vaccines and there are delays, you should be able to reach into your drawer, pull out a high-filtration mask, and feel protected. Not wear a bandana.
Right. Because respirators can provide protection against other airborne health threats, like wildfire smoke. They’re not just effective against viruses.
Oh, yeah, all kinds of stuff. I think the whole concept of cleaning the air is something that we have all sort of known, but didn’t take that seriously when it came to pollution and stuff like that. I think people are now starting to realize that the air we breathe is as important as the water we’re drinking or washing our hands.
How often can you reuse them? Does the electrostatic charge that attracts the particles wear off?
Peter Tsai, the scientist who invented the material used in N95s, has said that you could reuse them for a while and recommended buying seven masks and using a different one each day while letting the others sit out. Exactly how long the charge lasts, I think, really depends on the environmental conditions — humidity and sweat and things like that. But it’s up to the government to figure out how long an average person could use it. I think these are things that the CDC really should have been looking into. They’ve had a year and a half now. It’s crazy.
How has Omicron, which is clearly the most transmissible variant yet, changed your personal approach to managing your COVID risk, including when you decide to mask up outside of the hospital?
The transmissibility issue is a huge one, and masks are completely tied to that. The chances of catching COVID in transient or fleeting interactions, like being in the grocery store for a few minutes or being face-to-face with somebody for a conversation — I think it’s far more likely that I could get transmission now with this variant than with any others in the past. It changes my risk calculus.
I don’t think I’m going to get severely ill from this. I’m a healthy young guy, fully vaccinated. But I don’t want an infection for a few reasons. One is that I don’t want to transmit COVID to other people. Two, I don’t want to get infected at all. I can’t afford to be out of work. It’s the holidays, and the staffing isn’t great. I’m taking care of sick patients. Three, I don’t want to suffer potential morbidity effects, like long COVID and whatnot. I’ve treated and seen this in people that come in completely healthy, and they had ongoing symptoms for weeks after getting COVID. It’s real; I’ve treated patients who have this. We don’t know what to do with a lot of these cases.
And four, you don’t want to have a lot of infections at once. The problem with this high transmission is that you don’t want to surge. Surges are inherently bad. So when people are saying, “Well, I’m going to get this at some point anyways,” my response is that that may or may not be true, but it’s not good for everyone to get this at the same time. Because you may need to be evaluated in an emergency room, and people are still getting sick with other things that they had. And now some of those people are scared to go to hospitals, and they are getting delayed care for things that need urgent attention. There’s a lot of ripple effects from a lot of people getting sick at once. So, for me, it’s a no-brainer: This is not the time to increase your risk-taking.
What do you see as primary barriers when it comes to widespread public adoption of high-filtration masks?
I think that people don’t know which masks to get, or where to get them, and then actually being able to afford them. Those are issues that the government can address. They can literally just say, “Okay, let’s look into this. Here are four or five mask options that we think the public can use. Here’s an instructional kit on how to improve fit.”
It’s not going to be perfect, but we’re not aiming for perfect; we’re aiming for good enough to get transmission curbed significantly. Make these masks ubiquitously available. Make them available before you enter malls, before you enter grocery stores. Make them available in vending machines for a very low cost or no cost. Send some to people’s houses. There are so many ways to do this. It’s the job of some people in the government to figure these problems out. This is not my job. I’m in infectious disease taking care of patients; I’m not supposed to be telling the government how to do this. This is ridiculous.
Right.
I mean, these are operational problems. This is not even my expertise. I’m a doctor.
And this is not the first time you and others have tried to raise awareness about the need for better masks during this pandemic. It happened after Delta emerged, too.
It has come up like five different times. And let’s say it’s later, a different virus — do you want to be reaching into your underwear drawer again for a mask next time? This is ridiculous.
Another concern people seem to have about wearing better masks is fit. This seems to have always been the issue with surgical masks, which I rarely see anyone wearing correctly — tight across the mouth and nose with no open gaps. I know my beard, as illustrated by that periodically viral CDC infographic, reduces the protection my masks provide. I’ll sometimes buzz it down to try to get a tighter seal with my N95 when I know I’ll be going into a higher-risk situation. But while somebody with a big beard might think, What’s the point?, an imperfectly fit N95 is still better protection.
Exactly. And I’ll tell you, I feel completely protected now. I wore an N95 to the gym and worked out, and everything felt totally fine. I didn’t have any issues breathing. I felt protected. From day one of this pandemic, if you wanted to not shut down and you wanted people to still go into workplaces, there have been ways to do this. You can wear a good mask, go to work and then if you need to take a break, step outside. There are ways to do this and not have people bring the virus back home and infect their families.
To me, if you lose a few percentage points of efficacy here or there, that kind of pales in comparison to if everybody had better masks on, even if those masks were not completely, perfectly fitted or perfectly working at 95-plus efficacy. Even if they were working at 80 percent, if everybody was doing it, compared to 20 percent, it would still have such an immense impact on stunting transmission. That is the big picture here. People who argue, “Well if it’s unfitted, it may not be 95 percent effective,” are missing the forest for the trees.
Editors’s Note: Dr. Karan has also criticized a comment CDC director Rochelle Walensky recently made in which she said that while KN95 and N95 masks offer more protection, they “are often not as comfortable” and that might make people less likely to keep them on:
How do you and other health-care workers, in a higher-risk environment like a hospital, make sure your N95s fit properly?
We get fit tested once in the beginning of the year and then we don’t have a required fit test daily or anything after that. You use the mask that you’re fit-tested with and then you basically want to make sure that you don’t have facial hair, that you have a tight seal, and that your nose bridge is tightened in. And then, if you are feeling a lot of air coming out, you have to possibly readjust it. I haven’t had that happen yet though. My fit has never felt compromised with the mask I’m fit-tested for. And even with the masks I’ve used that I’m not fit-tested for, outside the hospital, it feels fine. I don’t feel any air leaking. It feels like a tight solid fit.
I’ve seen hundreds of cases, and I’ve never tested positive, let alone developed actual symptoms or gotten sick. So I really believe in the efficacy of these masks. And I believe health-care workers shouldn’t just be wearing them for patients with confirmed COVID, because during surges there’s a lot of occult transmission. So you have people who are testing positive that didn’t come in with COVID or didn’t test positive when they first came in, and you have a lot of community transmission that’s coming into hospitals from health-care workers and staff. So right now, during the surge, I am wearing my N95 when we go to the wards for all patients.
Studies seem to show that ventilation can have a larger effect than masking does, what do you make of that?
At a community level? Yeah. Ventilation has a uniform effect where you’re cleaning the air out. The difference is if you’re extremely infectious and someone’s right in front of you, it doesn’t matter unless you’re outdoors — ventilation is not going to be sucking particles out constantly to the extent that you’re going to completely stop transmission. Whereas if you’re wearing a mask in those closed settings, it would. And I think it’s an additive effect. All of these interventions are building upon one another to help. And so I think it’s not one versus the other.
Update: On January 14, the CDC finally updated its guidance on face masks to emphasize that high filtration respirators like N95s provide better protection against COVID transmission than cloth masks.
This interview has been edited and condensed for clarity, and has been updated.
The Strategist’s guide to face masks includes recommendations for multiple NIOSH-approved N95 respirators, as well as good KN95 and KF94 masks — which come in smaller sizes for children — and advice on how to avoid counterfeits.